4 Tips for Planning Successful Imaging Room Renovations
Dec 01, 2015

With today’s remarkable advances in technology, physicians are using imaging rooms for procedures that used to require an operating room. These breakthroughs are great for patient care and recovery.
But adding new functions to existing spaces can also present unexpected challenges. Hospitals can find themselves in situations like these:
- In a room designated as “Imaging,” a doctor now carries out procedures that use both imaging and anesthetic gas. During a survey, The Joint Commission flags the space function as a violation.
- A hospital is renovating an imaging-only room to include invasive procedures. The design team informs the hospital that they’ll need to upgrade the room’s ventilation – and the cost is beyond what the hospital had budgeted.
Why is this happening? The answer lies in the applicable codes and standards, and their need to keep up with rapidly advancing medical technology.
When updating imaging rooms, here are four tips for compliance, patient well-being, and effective space planning.
1. Check out ASHRAE Standard 170’s New Definitions for Procedures and Space Functions
ASHRAE Standard 170 lays out the requirements for ventilation of healthcare facilities. This fall, an important addendum to ANSI/ASHRAE/ASHE Standard 170-2013 (the formal name of the Standard) was released.
Addendum G finishes coordinating the Standard’s terminology for ORs and procedure rooms with the 2014 FGI Guidelines, so everyone is speaking the same language. Addendum G is available as a free download on the ASHRAE site.
The Addendum eliminates the terms “procedure room (Class A surgery),” “operating room (Class B surgery),” and “operating room (Class C surgery).” It adds definitions for these important terms:
- Invasive procedure
- Operating room (OR)
- Procedure room
- Restricted area
The definitions have a direct impact on facility design and operation, because hospital ventilation requirements are based on space functions. Which brings us to the second step.
2. Recognize How Space Functions Impact Ventilation Requirements
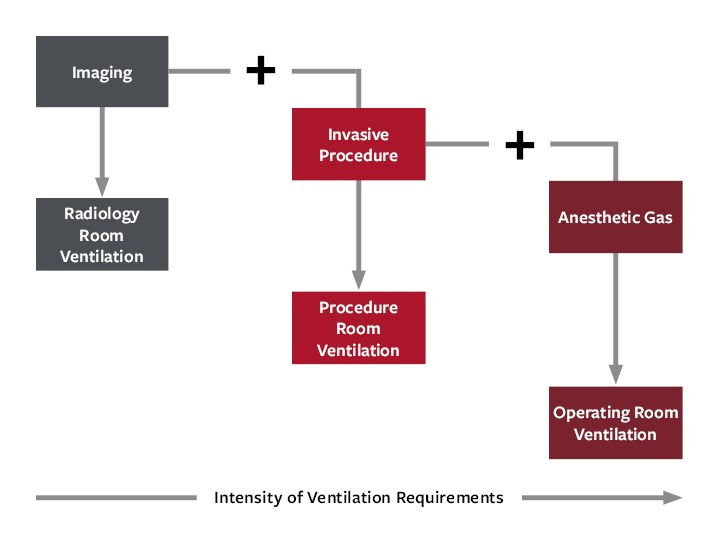
When the space functions change, the ventilation requirements change, too. This can dramatically impact infrastructure requirements. As the following diagram illustrates, HVAC requirements intensify as you add functions to a room.
Here’s a brief explanation of each:
A. Imaging
If a room is only being used for imaging (such as X-rays or CT scans), then radiology room ventilation is sufficient.
B. Imaging + Invasive Procedure
When the room will be used for imaging and invasive procedures, then the HVAC requirements increase to procedure room HVAC.
The room will need to have positive air pressure and a minimum of 15 air changes per hour (ASHRAE Standard 170 Table 7.1). One filter bank is required (ASHRAE Standard 170 Table 6.4).
C. Imaging + Invasive Procedure + Anesthetic Gas
If the room functions include imaging and invasive procedures and anesthetic gas, then HVAC systems need to meet ventilation requirements for operating rooms. That means having positive air pressure and a minimum of 20 air changes per hour (ASHRAE Standard 170 Table 7.1), two filter banks (ASHRAE Standard 170 Table 6.4), and laminar flow diffusers.
As far as the Standard is concerned, there is no difference between having the anesthetic gas brought in bottles or having it piped into the room. This level of HVAC requirements does not, though, apply to rooms where patients are simply sedated with medication. The focus is on the presence of anesthetic gas.
In addition, the requirements for anesthetizing location ventilation in NFPA 99-1999 still apply, because the 2000 version of the Life Safety Code (NFPA-101) is currently used by The Joint Commission and others. Smoke purge exhaust is generally needed to meet this requirement.
3. Make Sure Project Budget and Schedule Account for Current Ventilation Standards
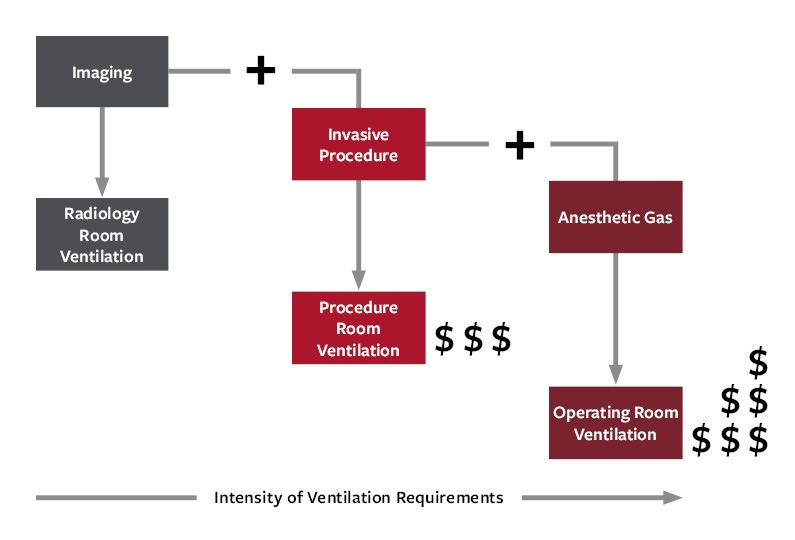
As the intensity of the ventilation requirements increases, the project cost also increases (assuming that the space doesn’t already have the proper ventilation in place).
Early in the planning process, it’s important to review existing infrastructure in light of the current standards. When you know what the standards require, along with what the space currently supports, you can form a more accurate estimate for the project budget and schedule.
Unfortunately, all too often we’ve seen project budgets and schedules set before a hospital is aware of the full project scope. That can leave the hospital scrambling to find extra funding, or having to tell physicians that the promised time frame or room functionality is no longer feasible.
4. Think about the Next 10 Years
A new piece of equipment may come with more functions than a hospital plans to use today. Imaging equipment, though, has a lifespan of 10 to 15 years. The question becomes, does the hospital expect to make use of those functions at some point in the next 10 to 15 years?
If the answer is “yes,” then it’s worth weighing the up-front cost of completing additional HVAC upgrades now against the down-the-road cost of taking a room out of service for upgrades.
Patient safety and code compliance are indispensable components of imaging room renovations. Knowing what the guidelines require, along with the impact to budget and schedule, helps decision-makers develop a comprehensive upgrade plan.